Healthcare is a battlefield as organizations compete for patient loyalty and market share. At the foundation, interactions with patients and their experience (e.g., a routine physical, a lab draw, a MRI study) must enhance the relationship that is cultivated between the patient and the clinician (e.g., physician, advanced practice provider, nurse, medical assistant). The entire care delivery team must be aware of the barriers to establishing this relationship and be empowered to implement change that creates a differentiated experience. This ultimately creates a brand recognition in local and regional markets that results in organic growth through reputation and word of mouth. In turn, your organization operates efficiently and creates a culture of professional fulfillment for you and your team.
Change Management – Transforming an organization and its operations is no small feat. To 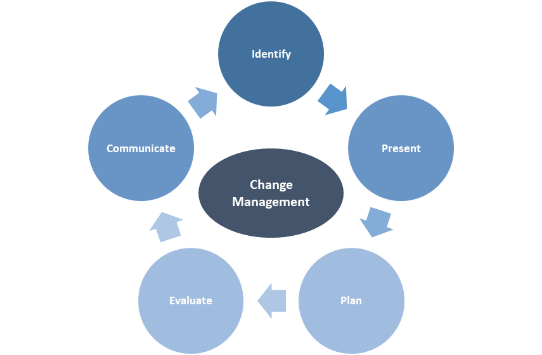 fundamentally improve performance, you must overcome the fear to change that is inherent in most human beings to seize opportunities or address key issues. Changes may include organizational redesign, roles and responsibilities, or deployment of technology. Ensuring your organization has an effective process to prepare, equip, and support individuals to successfully adopt change and drive organizational success is paramount to any performance improvement (PI) project.
fundamentally improve performance, you must overcome the fear to change that is inherent in most human beings to seize opportunities or address key issues. Changes may include organizational redesign, roles and responsibilities, or deployment of technology. Ensuring your organization has an effective process to prepare, equip, and support individuals to successfully adopt change and drive organizational success is paramount to any performance improvement (PI) project.
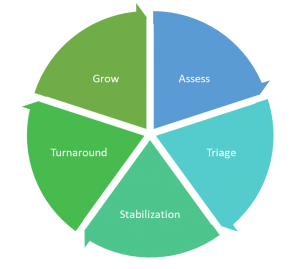
Financial Turnaround – The root cause of poor financial performance is often inherent in inefficient revenue cycle and/or expense management processes. Employing an analytic approach to determine the root cause of financial distress is a critical step to ensure you address the underlying reason for economic hardship. Addressing the wrong issue can have unintended consequences that further erode financial performance. Turnaround must focus on a complete review of both revenue and expense cycles.
Workflow Optimization – Whether you are eliminating redundancy (e.g., dual data entry), adding
capabilities (e.g., taking risk, capturing new clinical data, implementing a new EHR), or achieving a new outcomes (e.g., creating a new practice), changes to workflow are required. Inefficiencies result from regulatory and compliance complexities, varying reimbursement methodologies, prior authorization processes, and a host of other rules that administrative and clinical teams must abide by. For example, EHR technology promised efficient workflows for clinicians, however, were designed around payment methodologies which created inefficient clinical workflows. Organizations must break down processes into discrete units and reassemble those units into efficient processes to eliminate redundancies. In turn, this saves clinician time and allows the care team to focus on the relationship with the patient.
Technology Selection, Contracting, and Implementation – Evaluation of any technology requires a 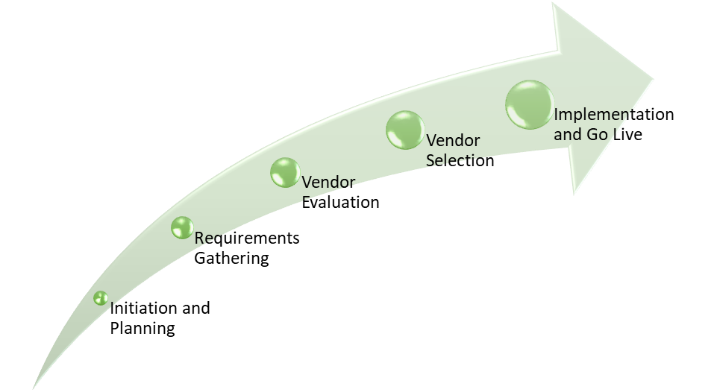 disciplined approach whether proactively evaluating new technology or evaluating a technology that is presented to you. The process starts with determining your end-state and the minimum requirements to accomplish that goal. Next, a quantitative review and comparison of those requirements against the best in class products is required to effectively evaluate alternatives. Contract negotiations must contemplate terms to identify performance milestones of the technology to ensure the solution meets the identified requirements. The process does not stop there, workflow redesign and change management processes must be considered when defining your requirements, planning for implementation, and during go-live to leverage the full value/potential of any solution.
disciplined approach whether proactively evaluating new technology or evaluating a technology that is presented to you. The process starts with determining your end-state and the minimum requirements to accomplish that goal. Next, a quantitative review and comparison of those requirements against the best in class products is required to effectively evaluate alternatives. Contract negotiations must contemplate terms to identify performance milestones of the technology to ensure the solution meets the identified requirements. The process does not stop there, workflow redesign and change management processes must be considered when defining your requirements, planning for implementation, and during go-live to leverage the full value/potential of any solution.
Interim / Project Management – We are available to assist with implementation efforts, either in interim management positions to fill vacancies or to augment your current management team.
The Process
At the heart of any PI initiative is a defined process that starts with an understanding of the end in mind. Asking the question, “What are the desired results and what are the barriers to achieving those results?” must always start the process.
Regardless of the methodology applied (e.g., Lean, 6-Sigma, PDSA cycles), there is no once size fits all. The inherent foundation of any PI initiative is cultural change that includes four major steps:
- Define – Articulate the desired
 outcome or end-state and identify the key performance indicators (KPIs).
outcome or end-state and identify the key performance indicators (KPIs). - Measure – Identify the gap between desired end-state and current-state for each KPI.
- Redesign – Isolate the root cause(s) driving the gap between end-state and current-state performance. Build process changes to solve for the root cause(s), garner stakeholder buy-in, and implement new workflows.
- Monitor (Real-Time) – Create dashboards to continuously monitor performance and ensure desired results are achieved and maintained.
Reinvest Health partners with senior leadership to implement controls to ensure effective change management methodologies guide your transformational efforts. We brings experience from all (PI) methodologies, including black-belt certification, to develop the best approach to solving our client’s performance related challenges.
