On the Brink: Restoring the Patient-Physician Relationship Part III
Our first and second installments of the series, On the Brink: Restoring the Patient-Physician Relationship, emphasized the vital importance of the relationship and the soft skills sets required to build trust and a bond between patients and physicians.
We take this opportunity to look at structural impacts to the patient-physician relationship, including healthcare financing, technology, and physical space. These areas represent opportunities to further enhance the patient-physician relationship.
Our healthcare system is the byproduct of economic and political influences around making healthcare affordable. Whether the beginnings of health insurance with teacher unions in Dallas, Texas in the 1920s[1], to significant changes in the way we pay for healthcare, the following events introduced influences on the patient-physician relationship:
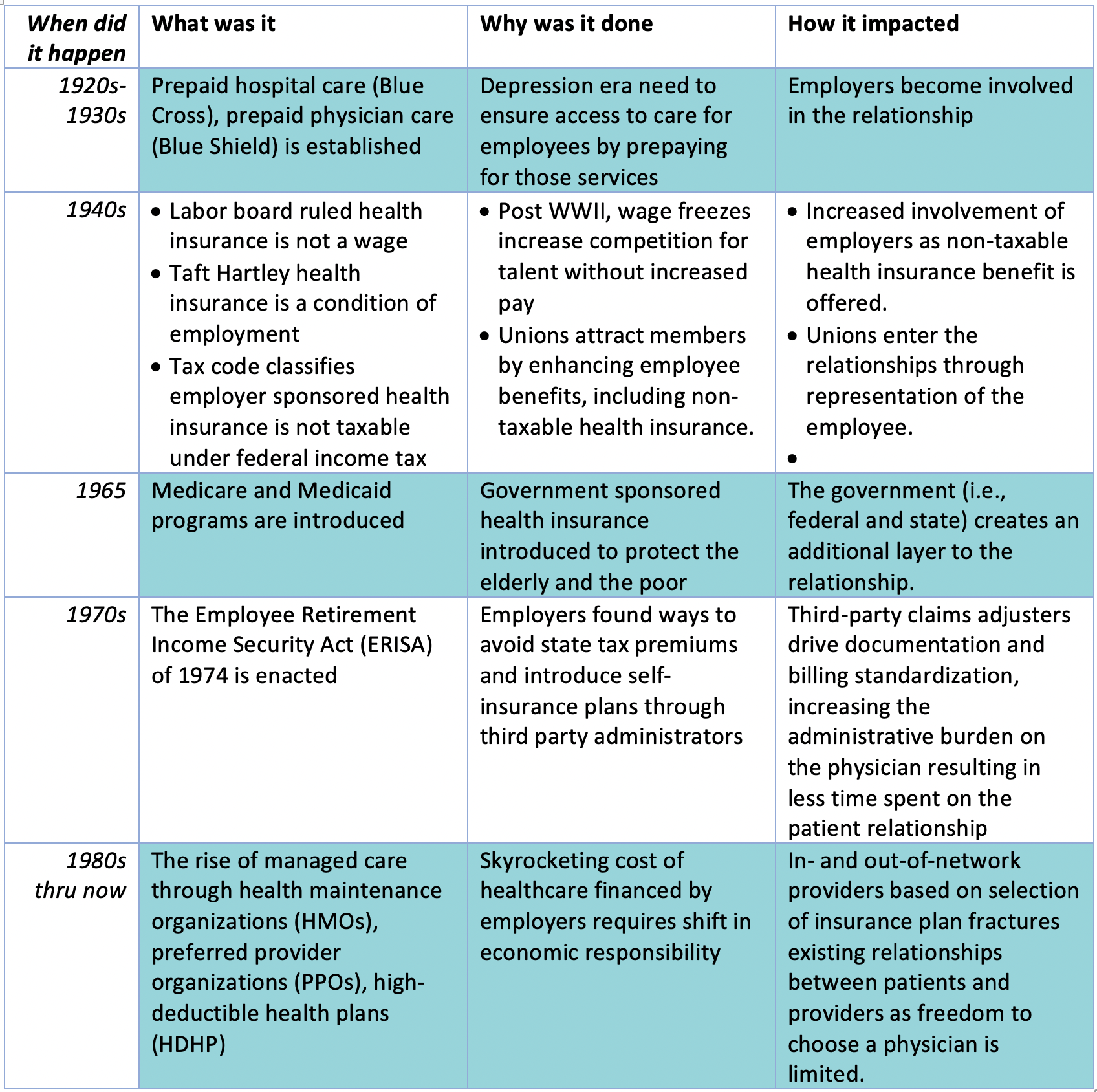
The unforeseen impacts of these financing related changes as additional stakeholders influence the clinical decision-making between the patient and physician is compounded by additional barriers, including but not limited to:
- Billing, collecting, and coding: Third parties, (insurers, employers, government) who are collecting premiums need to understand the costs of care. Systems for submitting/adjudicating claims and issuing/receiving payments become an essential administrative service of the medical practice and requires standardization across various insurance products/companies. Enter medical coding for services rendered (Current Procedural Terminology [CPT]) and justification for those services (International Classification of Diseases [ICD]).
- Verification of benefits, authorizations: A focus on cost containment requires predictability of care-related spend to reduce current and future-related expenses. To manage the predictability, third party payors introduced verification of benefits and pre-authorization of expenditure processes, thereby increasing the administrative and documentation processes that interfere with the patient-physician relationship.
- Technology and Electronic Health Records (EHRs): A need for efficient submission of documentation to justify healthcare expenditures, coupled with the advancement of technology introduced practice management and (EHRs) systems. The digitization of data allowed insurance carriers and government to compare providers’ (e.g., physicians, hospitals) cost and quality of care. Born were quality reporting requirements and mandatory implementation of EHRs designed to capture documentation rather than aid clinicians in the problem-solving and decision-making processes required to re-establish or maintain their patients’ health. Ironically, one of those quality measures is patient satisfaction with their physician.
- Increased patient volume to maintain income: The changes in workflows and incremental costs associated with these technologies further strained resources (e.g., operating margins, staffing) which required physicians to increase patient volume to bolster their revenue, resulting in decreased appointment durations with individual patients, prolonged wait times to be seen by the physician, and increased paperwork. These effects reduced the actual face-time between patient and physician, allowing less time to problem-solve and create goals for re-establishing or maintaining health.
- Offices become factories: The resulting technology, volume requirement and workflows dramatically changed the functionality of the physical office. Increased square footage associated with waiting rooms, triage areas, large banks of exam rooms, clinical coordination/scheduling offices, dedicated check-in and check-out queues are just some of the functional spaces required in a physician office space today
These factors continue to endanger and over-burdened the patient-physician relationship. However, we argue it is not too late to act even faced with the finance, technology, and physical challenges in place today. Building on trust and transparency as major components of healthy relationships, transparency and honesty are required in interactions among the various stakeholders who have been inserted in the relationship over the past century. The table below initiates the dialogue and actions required to bolster the relationship and reverse the trend.
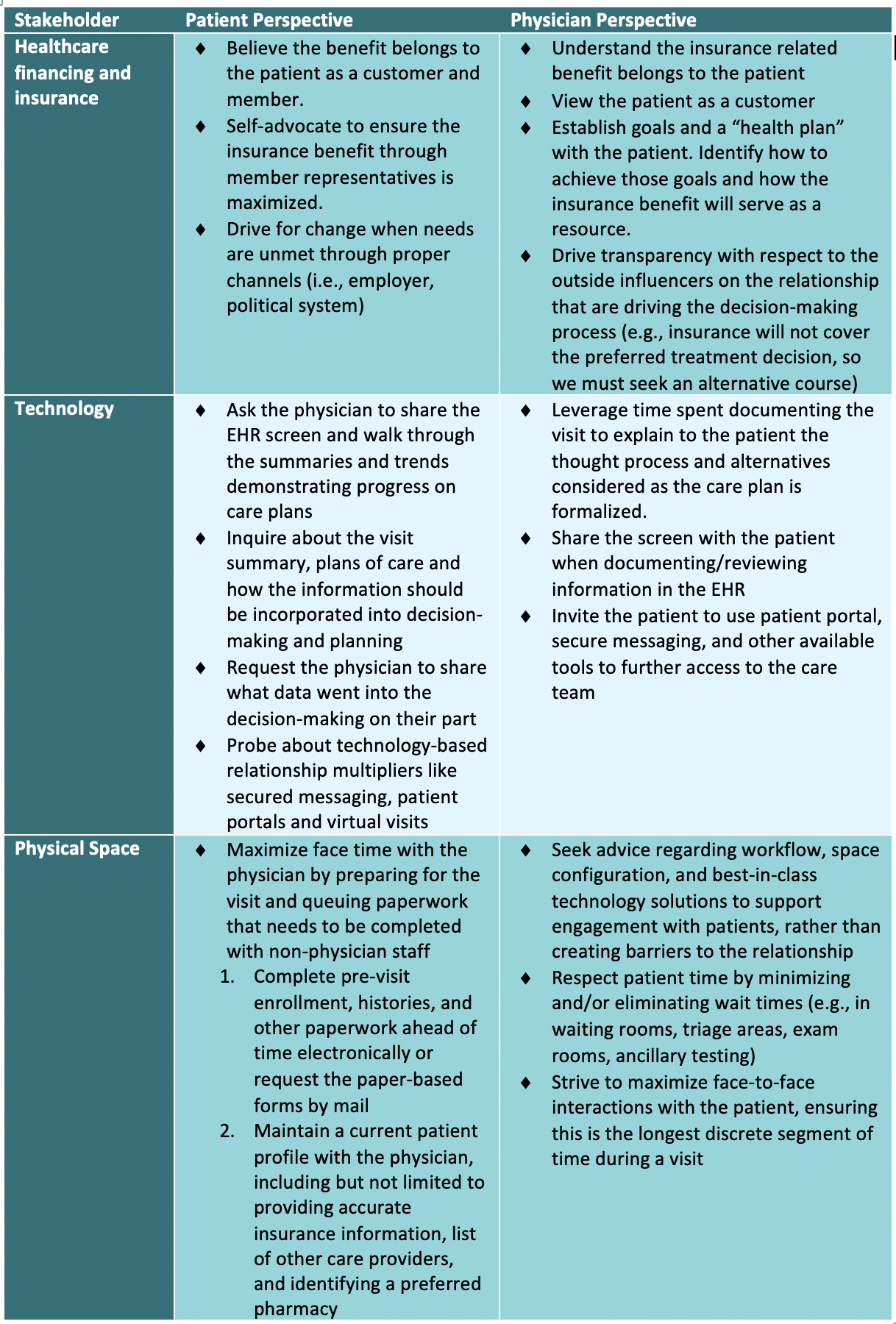
Understanding, shared empathy, and intentional actions can accomplish two things:
- On their own, leveraging these three soft skills build stronger relationships.
- These intentional actions must be applied to the influencers of finance, technology, and physical space to define financial and operational changes. These changes drive the future of healthcare delivery and will remove the barriers to allow the patient and physician relationship to thrive.
Look for our final post next week where we will explore an idealized healthcare system that focuses on optimizing the patient-physician relationship. We will identify the necessary macro level change(s) that must occur achieve the ideal healthcare system and the interim actions to employed to along the journey.
Please following Reinvest Health on LinkedIn® and share your thoughts on our blog series.
[1] https://www.ahpcare.com/a-brief-history-of-private-insurance-in-the-united-states/

