On the Brink: Restoring the Patient-Physician Relationship Part IV
In the first three installments of our series, On the Brink: Restoring the Patient-Physician Relationship, we emphasized the vital importance of the relationship between patient and provider, shared the soft skills sets required to build trust and a bond between patients and physicians, and highlighted the structural impacts that have a potential to create a barrier to the relationship. In our fourth and final part of the series, we examine the macro environment impacting the relationship and present foundational changes required to restore the patient and physician relationship, resulting in cost, outcomes, and satisfaction improvements.
Indeed, cost is a major driver of healthcare policy, employer benefit design, and increasing calls for universal healthcare. In our previous post, we detailed the physician-office activities that result from payor requirements to justify medical decision-making and secure reimbursement from third parties. These activities have a detrimental impact on the patient/physician relationship. The Annals of Internal Medicine estimates the administrative burden associated with insurance payor requirements amount to 34% of the total US healthcare expenditures in the United States (David U Himmelstein, 2020)[1].
 Therefore, we believe the administrative costs and burdens associated with third-party payor requirements must be eliminated given they do not add value and represent over one-third of the healthcare spend in our country.
Therefore, we believe the administrative costs and burdens associated with third-party payor requirements must be eliminated given they do not add value and represent over one-third of the healthcare spend in our country.
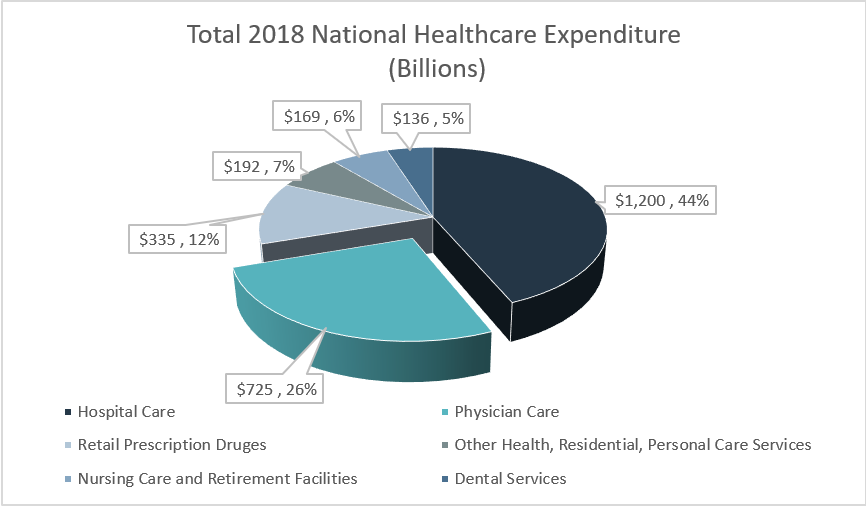
The Centers for Medicare & Medicare Services (CMS) National Health Expenditure Data reports a breakdown of the sources of our overall healthcare expenditures. A summary of this breakdown for the most recently reported year (i.e., 2018) is presented in the graph below[2]:
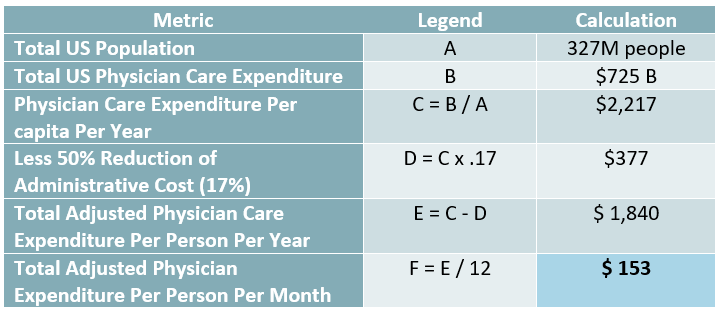
As we breakdown the healthcare costs associated with physician care on a per capita basis, we find roughly $150 per person, per month is spent. The table below summarizes our calculation.
This raises an important question: Is it possible to restore the patient/physician relationship without eliminating the interference from the third-party payor requirements that currently exist?
In short, it is not possible. We believe the optimal environment to nurture the patient/physician relationship must include a direct economic responsibility between the two parties with no interference from third parties. For skeptics that believe physician care is not affordable, we submit $150 per person per month is being spent today and could be redirected to individual pockets.
To draw an analogy, let’s look to the world of gambling. Casinos separate the “gambler”, or player, from their money by exchanging currency into chips. In this way, the gambler is not equating each transaction (i.e., bet) to real dollars. Likewise, a third-party payment token (i.e., insurance card) separates the patient, to varying degrees, from their money even in the face of co-pay, coinsurance, deductible and other out-of-pocket expenses. There is little to no economic consequences to the patient. Similarly, a gambler is disassociated from their money to varying degrees until they visit the cashier to exchange tokens for cash, assuming they have chips left. Conversely, the patient visits the check-out desk and is rarely asked for cash.
In conclusion, returning to a direct economic connection between patient and physician will further promote the relationship between both parties. Several attempts to increase the financial responsibility of the patient in an effort to create the economic connection and engage the patient in the decision-making have been made through the introduction of Healthcare Savings Accounts (HSAs) associated with High Deductible Health Plans (HDHPs). However, this has mainly resulted in cost shifting of a higher proportional spend and higher deductibles directly to the patient. Further attempts, driven by innovation by physicians, not insurance plans/employers, include variations on a membership medicine model, mainly Concierge Medicine and Direct Primary Care (DPC). Both models charge a monthly or annual membership fee in exchange for a higher level of access to a primary care physician. The main distinction is DPC practices do not accept insurance (eliminating the administrative burden) and therefore charge a lower membership fee, while Concierge Practice tend to charge a higher membership fee and do accept insurance.
We will explore these models and discuss the benefits and limitations in future posts. The key takeaways of our four-part series are as follows:
- The relationship between patient and physician is sacrosanct and must be the foundation of healthcare redesign in this country.
- The barriers to forming a strong bond between patient and physician must be identified and eliminated to allow the relationship to flourish.
- Administrative burdens and interference in the clinical judgement of the physician and the shared decision-making with the patient must also be eliminated.
- Physicians must focus on quality, not quantity and decrease their “patient panel” sizes to ensure they provide adequate time to their patients to nurture the relationship with their patients, build plans to restore/enhance health, and introduce processes to hold patients accountable to their goals.
We hope you have enjoyed this blog series and invite you to the conversation. Please share your thoughts and positions on this topic and follow us on Linked In!
Works Cited
A Brief History of Private Insurance in the US. (2020, March 18). Retrieved from Academic Health Plans: https://www.ahpcare.com/a-brief-history-of-private-insurance-in-the-united-states/
Allegheny County Medical Society. (2019, August 27). Direct Primary Care: A win-win for doctors and patients. Retrieved from Allegheny County Medical Society: https://www.acms.org/2019/08/direct-primary-care-a-win-win-for-doctors-and-patients/
CMS.gov. (2019, 12 17). NHE Fact Sheet, Historical NHE, 2018. Retrieved from CMS.gov: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet
David U Himmelstein, M. T. (2020, January 21). ACP Journals. Retrieved from Annals of Internal Medicine: https://www.acpjournals.org/doi/10.7326/M19-2818
Reynolds, K. A. (2019, October 9). New study estimates U.S. Healthcare waste costs nearly $1 trillion each year. Retrieved from Medical Ecomics: https://www.medicaleconomics.com/view/new-study-estimates-us-healthcare-waste-costs-nearly-1-trillion-each-year
[1] (David U Himmelstein, 2020)
[2] (CMS.gov, 2019)

